Cerebral Palsy from Hypoxic-Ischemic Encephalopathy (HIE)
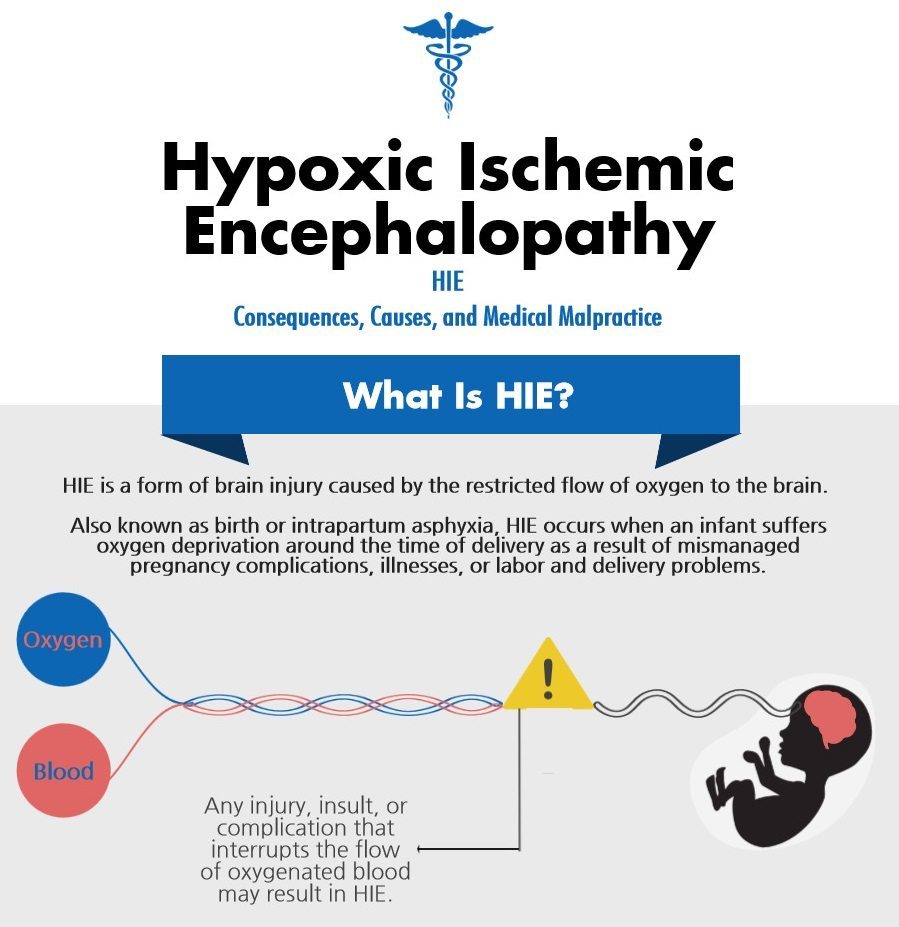
Hypoxic-ischemic encephalopathy (HIE) is a type of neonatal brain injury that occurs when a newborn receives insufficient oxygen to the brain around the time of delivery. Also known as intrapartum asphyxia, neonatal encephalopathy (NE), or birth asphyxia, hypoxic-ischemic encephalopathy is one of the most common forms of brain injury caused by fetal oxygen loss. Hypoxic-ischemic encephalopathy / HIE may occur as the result of a number of mismanaged pregnancy, labor, and delivery issues, and the dangerous brain injury often leads to lifelong brain damage, developmental delays, and cerebral palsy (CP).
Was your child diagnosed with cerebral palsy (CP) or another permanent disability as the result of hypoxic-ischemic encephalopathy / birth asphyxia? If so, you and your child may have grounds for a medical malpractice claim. We encourage you to reach out to our Michigan hypoxic-ischemic encephalopathy (HIE) lawyers with your legal questions today. Our team of Michigan HIE lawyers will provide you with a free case review and inform you of your legal options. Should the birth injury lawyers at Michigan Cerebral Palsy Attorneys take your hypoxic-ischemic encephalopathy case, you will not be charged until they win or settle in your favor. You may reach our Michigan hypoxic-ischemic encephalopathy (HIE) lawyers 24/7 in one or more of the following ways:
- Call Michigan Cerebral Palsy Attorneys toll-free at (888) 592-1857
- Live Chat with Michigan Cerebral Palsy Attorney by pressing the Live Chat tab on the left of your screen
- Complete our online contact form here
What Injuries Are Associated with HIE?
The extent of a child’s asphyxia around the time of birth dictates how severe the consequences of intrapartum asphyxia will be. While infants’ bodies can handle oxygen limitations for short periods of time, extended asphyxia destroys brain tissue and can result in varying degrees of brain injury. Hypoxic-ischemic encephalopathy may result in the following lifelong injuries:
- Cerebral palsy
- Seizures: Hypoxic-ischemic encephalopathy is the leading cause of seizures in newborns.
- Epilepsy
- Motor function delays
- Neurodevelopment impairments
- Cognitive disabilities: A number of babies sustaining birth asphyxia brain injuries develop intellectual disabilities because oxygen deprivation around the time of birth may hinder a child’s intellectual and adaptive functioning.
- Death
What Causes Hypoxic-Ischemic Encephalopathy (HIE)?
-
Delayed emergency C-section: If a baby exhibits signs of distress, medical professionals must perform an emergency C-section immediately to avoid cutting off oxygen to the baby.
- Pitocin and Cytotec: Hyperstimilation is a complication of the labor induction drugs Pitocin and Cytotec that limits the flow of oxygenated blood through the umbilical cord, thereby restricting oxygen to the baby.
- Prolonged and arrested labor: Labor is traumatic for the baby, and prolonging its forces and pressures often leads to fetal oxygen deprivation, particularly in cases where Pitocin and Cytotec are used.
- Uterine rupture: Tearing of the uterus can limit oxygen to the baby in two ways—for one, the mother may lose so much blood that blood flow to the baby is restricted, and secondly, the rupture may cause the placenta to separate from the mother’s circulation (thus diminishing the flow of oxygenated blood to the baby). Vaginal births after Cesarean (VBAC) put mothers at increased risks for uterine rupture.
- Placental abruption: When the placenta separates from the uterus, abruption can limit oxygen to the baby.
- Abnormal fetal size and malpresentation: Size or presentation abnormalities often result in prolonged labor, which can cause brain bleeds, trauma, umbilical cord prolapse and compression, all of which may result in fetal asphyxia. The following are examples of size and presentation abnormalities that can cause hypoxic-ischemic encephalopathy:
- Cephalopelvic disproportion (CPD): CPD is a complication in which the baby’s head is too large to pass through a mother’s pelvis.
- Breech presentation: A birth presentation where baby’s feet or buttocks enter the birth canal first.
- Macrosomia: A condition in which the baby is larger than average for his or her gestational age.
- Umbilical cord problems: The umbilical cord is the baby’s lifeline, so interferences with its functions often cause fetal asphyxia.
- Umbilical cord prolapse and compression: Prolapsed cords enter the birth canal before the baby, often putting pressure on the umbilical cord and limiting oxygen to the baby.
- Nuchal cords and true knots: When the umbilical cord wraps 360 degrees around a baby’s neck, oxygen flow is restricted.
- Short cord: Movement within the womb promotes fetal growth, so short cords result in the many complications associated with growth restrictions, such as HIE.
- Preeclampsia: Pregnancy-induced maternal high blood pressure constricts placental blood vessels and can decrease blood flow to the baby.
- Placental previa: Sometimes the placenta grows so close to the opening of the uterus that it may partially or completely block the opening of the birth canal. Its complications often result in fetal oxygen deprivation.
- Post term pregnancy: After 37 weeks, the placenta and uterus begin to deteriorate and less oxygen-rich blood reaches the baby.
- Uteroplacental insufficiency: Anything that results in insufficient blood flow to the placenta during pregnancy leads to fetal oxygen deprivation and hypoxic-ischemic encephalopathy.
- Polyhydramnios: Excessive amounts of amniotic fluid increase the likelihood of cord prolapse, placental abruption, and premature birth, all of which may lead to oxygen deprivation.
- Oligohydramnios: Insufficient amniotic fluid typically denotes placental insufficiency, cord compression, fetal growth restriction, preeclampsia, and placental abruption, which all may lead to fetal oxygen deprivation.
- Premature rupture of membranes (PROM): Premature rupture of the amniotic sac and chorion can lead to infection and preterm birth, both of which often result in oxygen deprivation.
- Anesthesia mistakes: interfere with maternal and fetal oxygen intake directly affect how much oxygen reaches the baby.
- Fetal stroke: Fetal stroke greatly increases the chances of hypoxic-ischemic encephalopathy. Fetal stroke, which occurs when blood vessels in the brain become blocked or restricted, often results from blood clots, decreased placental blood flow, high or low blood pressure in the mother, weakened blood vessels, pelvic inflammatory disease (PID), or other maternal infections.
- Intracranial hemorrhages (brain bleeds): Traumatic delivery or deliveries necessitating the use of vacuum extractors or forceps can cause head trauma that may result in HIE.
- Improper management of a baby’s respiration after birth
- Improper management of anemia (low red blood cell count) after birth
- Fetal monitoring errors: When medical professionals fail to correctly interpret fetal distress through fetal heart tracings, they risk missing the emergency situations (like oxygen deprivation) that require intervention.
- Premature Birth: Since a neonate’s lungs mature between 32 and 34 gestational weeks, premature babies without proper medical assistance lose oxygen flow to the brain and face the risk of hypoxic-ischemic encephalopathy.
The Three Types of Birth Asphyxia
The types of injuries that cause birth asphyxia typically fall into three different categories. Below, we’ll discuss those categories and list a few obstetrical complications that can lead to hypoxic-ischemic encephalopathy.
- Acute Near Total Asphyxia (or acute profound asphyxia) is the most extreme form of HIE. In cases of acute profound asphyxia, the infant generally suffers complete, severe, or extended oxygen deprivation from obstetrical complications including uterine rupture, umbilical cord prolapse, umbilical cord compression, placental abruption, terminal bradycardia, and vaginal birth after Cesarean (VBAC) issues.
- Partial Prolonged Asphyxia is the second most severe type of hypoxic-ischemic encephalopathy. When partial prolonged asphyxia occurs, the oxygen deprivation usually lasts for around a half hour. Common causes of partial prolonged asphyxia include abnormally high amniotic fluid levels (a condition known as oligohydramnios), preeclampsia, failed resuscitation of a newborn after delivery, hypertension, hypotension, strong contractions, uterine hyperstimulation, umbilical cord compression, placental problems, and nuchal cords.
- Mixed Injury Pattern Asphyxia blends elements of both acute profound asphyxia and partial prolonged asphyxia.
What Are the Signs and Symptoms of HIE?
 The baby requires resuscitation after delivery or at any time during the neonatal period
The baby requires resuscitation after delivery or at any time during the neonatal period- Low APGAR scores for longer than 5 minutes: An APGAR score assesses the overall health of a newborn over the first few minutes of life, and low scores often denote oxygen incidents or deficiencies.
- Seizures within the first 24 – 48 hours after delivery are an indication of HIE caused during delivery, and seizures while in the NICU or shortly after discharge from the NICU are an indication of an oxygen-depriving insult from delivery.
- Difficulty feeding
- Profound metabolic or mixed acidemia in an umbilical cord blood sample (the baby’s blood is acidic)
- Decreased muscle tone (hypotonia)
- Organ problems
- Absence of brain stem reflexes: For instance, breathing problems and an abnormal response to light
- Coma
How Is HIE Diagnosed?
Most of the aforementioned causes of HIE will trigger changes to the baby’s fetal heart rate monitor and alert physicians of the condition’s presence, prompting physicians to perform diagnostic tests. Additionally, certain signs of hypoxic-ischemic encephalopathy may appear after birth such as seizures and organ dysfunction. If there is any possibility that a baby suffered oxygen deprivation to the brain, it is crucial for the medical team to closely monitor the baby for signs of hypoxic-ischemic-encephalopathy. CT scans, PET scans, MRIs, blood glucose tests, arterial blood gas tests, EEGs, and ultrasounds can detect birth asphyxia, but in some cases, HIE may not become apparent until the child later exhibits developmental or motor delays.
How Is Hypoxic-Ischemic Encephalopathy Treated?
Since HIE results in lifelong brain damage, treatment is supportive. Children with hypoxic-ischemic encephalopathy can use therapies to adjust to mental and physical impairments. However, a procedure known as the “hypothermia treatment” has shown promising treatment results. The hypothermia treatment, which consists of lowering a newborn’s body temperatures, has been proven to reduce the severity of neurological injury. For the treatment to bear any results, physicians must quickly diagnose HIE and begin the hypothermia treatment. By reducing a newborn’s temperature to roughly 91 degrees Fahrenheit for 72 hours, the process is able to slow metabolic rate and allow cells to recover. The three most important prerequisite conditions for hypothermia treatment include:
- The baby must be at least 36 gestational weeks old
- The oxygen-depriving insult must have occurred within a six hour time frame from the beginning of the treatment
- There cannot be any contraindications to the treatment
Video: The Importance of Fetal Monitoring in Avoiding HIE
In the following video, you’ll learn more about how errors related to fetal heart monitoring can cause fetal oxygen deprivation, fetal distress, and hypoxic-ischemic encephalopathy. Andrea Shea, our in-house registered labor and delivery nurse, explains the relationship between electrical fetal monitoring (EFM), medical malpractice, hypoxic-ischemic encephalopathy, cerebral palsy, and other birth injuries.
Legal Help for Hypoxic-Ischemic Encephalopathy / HIE and Cerebral Palsy in Michigan
Michigan Hypoxic-Ischemic Encephalopathy (HIE) Lawyers and Attorneys
 When a loved one is affected by cerebral palsy or another birth complication, parents or guardians have to meet expensive medical bills, attend time-consuming rehabilitation procedures, and cope with the accompanying emotional burdens. Unfortunately, birth complications from conditions like hypoxic ischemic encephalopathy are often the result of negligence on the part of a medical professional.
When a loved one is affected by cerebral palsy or another birth complication, parents or guardians have to meet expensive medical bills, attend time-consuming rehabilitation procedures, and cope with the accompanying emotional burdens. Unfortunately, birth complications from conditions like hypoxic ischemic encephalopathy are often the result of negligence on the part of a medical professional.
Instances of medical negligence that may cause hypoxic-ischemic encephalopathy include:
- Failure to identify signs of fetal distress and take fast and appropriate action; ignoring or misinterpreting fetal distress signs
- Failure to properly monitor and treat the mother and baby during pregnancy, labor, and delivery
- Failure to properly assess and test for the risks factors, causes, signs, and symptoms of hypoxic ischemic encephalopathy/birth asphyxia
- Failure to diagnose and treat maternal or fetal conditions or infections that lead to hypoxic ischemic encephalopathy and birth asphyxia
If you experienced these situations or similar instances of medical malpractice during your pregnancy or delivery, don’t hesitate to contact us:
We handle cases throughout the U.S.
Call our offices toll-free at (888) 592-1857
Press the Live Chat tab to the left
Complete this online contact form
Related Reading on Hypoxic-Ischemic Encephalopathy
Additional information on hypoxic-ischemic encephalopathy and our Michigan HIE law firm
- Information on HIE and Cerebral Palsy:
- Infographic: HIE
- Hypothermia Treatment & Hypoxic-Ischemic Encephalopathy
- Cerebral Palsy Information
- Hypoxic-Ischemic Encephalopathy (HIE) and Nuchal Cords
- Hypoxic-Ischemic Encephalopathy (HIE) and Seizures
- Hypoxic-Ischemic Encephalopathy (HIE) and Uterine Rupture
- Hypoxic-Ischemic Encephalopathy (HIE) in Twins and Multiples
- Hypoxic-Ischemic Encephalopathy (HIE) from the Misuse of Pitocin & Cytotec
- Our Law Offices:
- Blogs: